The woman was lying still on the floor of the ambulance when Emma Åkerlund opened the doors. Between her legs was a tangle of fabric with something inside — the body of a newborn boy with the placenta and umbilical cord twisted up in his mother’s skirt. If he survived the delivery, he did not last long after.
The woman was lying still on the floor of the ambulance when Emma Åkerlund opened the doors. Between her legs was a tangle of fabric with something inside — the body of a newborn boy with the placenta and umbilical cord twisted up in his mother’s skirt. If he survived the delivery, he did not last long after.
The woman had gone into labour earlier that day in November last year. But health workers feared that she had Ebola, and refused to treat her. She had spent hours alone in the back of the ambulance as it made its way to ELWA3, an Ebola management centre in Monrovia, Liberia, run by the medical aid group Médecins Sans Frontières (MSF).
Åkerlund, a gynaecologist and obstetrician, was able to examine the woman while wearing full protective gear: a waterproof body suit, gloves, boots and goggles. She asked the woman if she wanted to see her son; the mother declined. So Åkerlund zipped the baby into a body bag and sterilized it with bleach, just in case the mother and child were infected.
Tests performed later that day proved that they were not. There had been no medical reason for doctors and nurses to turn the woman away. And although there is no guarantee that the child would have survived with proper medical care, there was no reason for him to come into the world — and then exit it — on the floor of an ambulance.
“I’m not blaming anyone for not taking them in,” Åkerlund says. “It’s a huge problem to try to take care of pregnant women in an Ebola epidemic.”
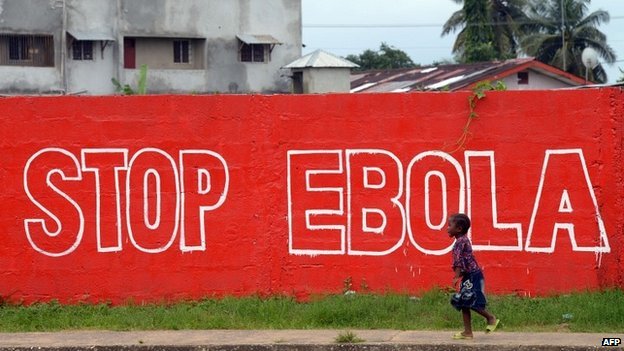
Ebola is having tremendous knock-on effects for maternal health in Liberia, Guinea and Sierra Leone. Pregnancy seems to make women uniquely vulnerable to the effects of the disease, and babies born to infected women have not been known to survive. Compounding these individual tragedies, the blood and abundant bodily fluid that accompanies delivery or miscarriage pose enormous risk of infection to health workers. As a result, many refuse to treat patients who are pregnant for fear that they will become infected. And throughout the region, fears about Ebola and stories about women being turned away have convinced many pregnant women to stop showing up for routine prenatal visits or for assistance with delivery.
The epidemic has so far infected more than 23,900 people, killing 9,700 of those, and although it is on the wane it is unclear when it will end. For maternal health, the effects are devastating. The United Nations Population Fund (UNFPA) estimates that, either directly or indirectly, the epidemic will result in as many 120,000 maternal deaths by the end of October.
Researchers, public-health experts and activists worry that this trend could undermine advances made in the region’s health, education and more. For instance, children whose mothers die may end up orphans and be forced to choose work over school. Teenagers have found themselves becoming family breadwinners.
“The impact on maternal and child health will be one of the most important and long lasting from this outbreak,” says Alexandre Delamou, chief of research at Guinea’s National Centre for Training and Research in Maferinyah.
Fearsome odds
Doctors are still trying to work out why Ebola is more deadly for some people than others. For pregnant women, the consequences of infection seem dire. In the first Ebola outbreak ever identified, in Zaire in 1976, 73 of 82 infected pregnant women died. In a 1995 outbreak in Kikwit, Democratic Republic of the Congo, researchers observed that all but one of 15 pregnant women treated at one hospital died.
Such samples are too small to say anything with certainty, but the idea that pregnant women would be more at risk of dying makes sense. Ebola increases the risk of haemorrhage, which is already elevated in childbirth. And pregnant women are more likely than other adults to die from several other infectious diseases because of a natural suppression of immunity that helps to protect developing fetuses.
The fetuses never seem to make it. In every case reported in the literature of a woman with Ebola giving birth, the baby has either been stillborn or died shortly thereafter. Why this happens is unclear; it could be because of the high viral load that crosses the placenta, because the virus is transmitted through breast milk or because mothers who are sick or recovering from Ebola are in no shape to care for newborn babies.
Pregnant women with Ebola also pose serious risks to caregivers. The symptoms of Ebola for a pregnant woman — abdominal pain, vaginal bleeding, premature labour, nausea, diarrhoea and vomiting — can be very difficult to differentiate from standard pregnancy complications. Given the high exposure to bodily fluids during delivery, those who guess wrong often do so at their peril.
About one-third of the medical staff who died from Ebola in Sierra Leone between April and September last year, for instance, were mother-and-child health aides. This group had a higher death rate than other types of health worker, such as doctors or nurses.
Amadu Jawara, a nurse and community health worker in Freetown, Sierra Leone, is one of the lucky ones. In November, he and Samuel Batty treated a pregnant woman with abdominal pain and a fever. Because the fever responded to medication, they assumed she had malaria and did not use full protective gear while examining her. But she soon worsened and later died of Ebola. Jawara and Batty were placed in isolation for 21 days. Batty died from the disease on 2 December; Jawara did not get infected.
“The Ebola epidemic may cause as many as 120,000 maternal deaths by the end of October.”
On the day he reported back to work, six women arrived at the hospital in need of Caesarean sections. Many doctors and nurses had abandoned their posts during the epidemic, and there were no surgeons available. Jawara, who had been trained in basic surgery, was the only person there to perform the deliveries. “They told me I should intervene,” Jawara says. “I had no choice.” He has since performed 100 such procedures.
The staff try to screen out patients who have a fever or demand that they take an Ebola test. But this leaves some women without care during labour, and some deliver on the floor of the waiting room with no one to help them. And screening is not foolproof.
On 13 January, Jawara saw a patient who had been four months pregnant but whose fetus had stopped moving. She had a low-grade fever, and Jawara admitted her, believing that she had an infection.
Two days later, she expelled her fetus and Jawara helped to deliver her placenta. The woman soon developed diarrhoea and a high fever. She tested positive for Ebola.
Jawara’s lucky streak continued; he did not become infected. But every episode like this deepens the fear that health-care workers have of treating pregnant women. Some worry that the rift between the two will outlast the epidemic. “Ebola will have an everlasting impact on the health system in Sierra Leone,” Jawara says. “The fear is still there.” Even as the epidemic winds down, many health workers remain absent from their posts.
Turned away
Researchers who study maternal mortality talk about the “three delays” that increase the proportion of women who die in childbirth: delays in deciding to go to a hospital, delays in getting there and delays after arriving caused by factors such as electricity cuts or the lack of a trained doctor. Ebola has exacerbated all three.
In September, a team of researchers led by the US Centers for Disease Control and Prevention (CDC), for example, interviewed pregnant women and health-care workers in Kenema, a town in southeastern Sierra Leone that was at the epicentre of the epidemic when it started in the country. They found that pregnant women stayed away from hospitals for fear of contracting Ebola, or because of rumours that health-care staff were injecting patients with Ebola, harvesting their blood for sale or misdiagnosing them with Ebola because they were paid extra for referring them to treatment units. Even after outreach workers conducted education campaigns in local communities, all of the 27 pregnant or breastfeeding women who participated in the study said that they knew of at least one person who was refusing to go to health-care facilities because of such rumours.
Many women who wanted to go to clinics were prevented from reaching them by quarantines, roadblocks or a lack of transportation. And those who made it were often turned away because the staff were afraid of getting infected. Many hospitals were formally or effectively closed because staff stopped going to work. In Freetown, the capital and largest city of Sierra Leone, the biggest public maternity hospital has been running on skeleton staff for much of the outbreak. In the second largest city, Bo, MSF closed one of the few programmes in the country that offered advanced surgical care for pregnancy complications last August. The decision came after several instances in which staff had difficulty diagnosing Ebola cases. It has still not reopened.
CDC researchers found from their surveys that education campaigns are helping to ease fears in regions of the epidemic that are no longer seeing many new cases. The immediate damage is nevertheless erasing fragile gains that these countries had made in maternal health.
Delivering change
Before the outbreak began, Liberia, Guinea and Sierra Leone had some of the world’s highest maternal death rates: in Sierra Leone, more than 1,000 of every 100,000 child births results in the death of the mother. That is hundreds of times the ratio for developed countries in Europe. But it actually represented a vast improvement from where Sierra Leone was near the end of its civil war in 2000, when the death rate was twice as high. Rates of death during childbirth had also dropped in Liberia and Guinea thanks to a combination of national governments declaring maternal mortality an important health priority, an influx of foreign aid and major public-health campaigns. The gains have been made despite a lack of trained medical professionals and the fact that these countries are some of the poorest on Earth.
“It’s like we had taken one step forward before Ebola and now we’ve taken three steps back.” says Shumon Sengupta, country director in Sierra Leone for Marie Stopes, a non-governmental organization that provides family-planning services. A study conducted on behalf of the UNFPA, for instance, modelled the impact of the reductions on routine care provided to pregnant women in Sierra Leone in the first six months of the epidemic. The preliminary work found that the cuts may have caused 20% more maternal deaths.
Now, the maternal death rate is projected to double to more than 1,000 per 100,000 live births in Guinea and Liberia and to more than 2,000 per 100,000 live births in Sierra Leone, returning to wartime levels.
“We think the collateral damage of the epidemic is higher than the damage caused by the epidemic itself,” says gynaecologist Séverine Caluwaerts, who works at the Institute of Tropical Medicine in Antwerp, Belgium, and with MSF.
The UNFPA is looking to convene a meeting to analyse the state of the science around reproductive health and Ebola and how to prevent such impacts during future outbreaks. A crucial issue is how to boost the survival of pregnant women who become infected.
MSF obstetrician Benjamin Black and his colleagues have designed a ‘maternity box’ containing all the supplies that caregivers would need to help prevent haemorrhage in cases in which the uterus fails to contract after delivery, a major complication that threatens pregnant women with Ebola. These supplies include drugs such as oxytocin and misoprostol, which encourage contraction, and a catheter to empty the bladder, which can speed up delivery.
The box spares caregivers from having to exit the patient area, take off their protective equipment and re-gown if they need something vital. Simple adjustments such as this have helped MSF to save the lives of 23 pregnant women with Ebola.
In January, MSF opened a clinic in the outskirts of Freetown that specializes in care for pregnant women with Ebola. The clinic has adapted its procedures to meet the additional risks in looking after these women — for instance, adding a third pair of gloves that reach the elbow to the standard two pairs. And staff try to avoid surgical procedures, such as episiotomies and Caesarean sections, that are too dangerous for workers and patients.
Åkerlund says that she is constantly thinking about how to protect herself and other staff so that they feel able to care for pregnant women rather than turning them away.
One case from her time in ELWA3 haunts her: an apparently full-term pregnant woman who arrived at the treatment centre without a single symptom of Ebola. She had thought that her waters had broken and she headed for the hospital but was turned away from multiple clinics by reticent staff. Åkerlund thought that the woman was another perfectly healthy mother-to-be who might lose her baby to nothing more than fear. She and her staff admitted the woman, brought her to a place where she could be kept separate from other patients and ordered an Ebola test.
Hours later, Åkerlund received the results: the test was positive. A second test was also positive. The woman was moved into the ward for confirmed cases on 26 November. Within days, her condition deteriorated; her blood stopped clotting, and her baby stopped moving. The following day, the woman died.
The case sticks in Åkerlund’s mind as an example of the dilemmas that confront both caregivers and pregnant women in an Ebola epidemic, when diagnostic tests can take hours or days and a woman in labour may need help immediately. But Åkerlund knows that giving up is not an option. “I don’t think the solution is to say you can’t do maternity care in an outbreak and leave these women without anything.”